Medically Necessary Directed Donation
Effective April 14, 2023, Carter BloodCare only offers medically necessary directed donations.
You may have seen a lot of social media discussion of late about the recent decision to drop our directed donation program at Carter BloodCare. The directed donor program was an option put in place in the 1980s when the fear of HIV in the blood supply was real, and allowed patients to choose their own blood donors from friends and family.
Since then, a lot has changed.
We have radically better blood screening processes, including vastly better blood testing. The confidence in the community blood supply has grown. Therefore, over the intervening years, the number of requests for directed donors has dropped significantly.
In order to maintain this program, we have had to have complicated processes in place to track these units. I often use the analogy of currency banking. If you deposited a $20 bill at a branch bank in Fort Worth and you said you wanted the exact same $20 bill back in two weeks at a different branch bank in Dallas, think about the logistics in making that happen.
Directed donations were made available for the psychological comfort of the patients and/or their families. Scientific literature has not supported any safety advantage of directed donations and often shows a disadvantage because of the preponderance of first-time donors with higher infectious disease markers (see references below). Individuals may present to donate under pressure from friends or family despite risk factors for infectious disease that they do not wish to disclose to their loved ones.
Other risks include using the blood of a husband for transfusion of a wife and putting her at risk of future hemolytic disease of the fetus/newborn.
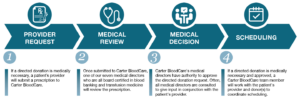
Carter BloodCare continues to maintain a program to collect and process units from selected donors on demand when medical need demands.
If a patient with a rare blood type or other unusual situation arises – such as transplant patient refractory to all banked blood other than their marrow donor, or mother who needs to donate to her infant with neonatal alloimmune thrombocytopenic purpura – and a specific donor is identified who meets the need, we can draw that donor for that specific patient.
The difference here from the directed donor program is that directed donors were at the patient’s request, not for medical need. The transfusing physician needs to order these units as medically necessary from those donors. Otherwise, the community blood supply is there to serve our patients as needed.
Our highly skilled and experienced blood typing laboratory at the main Carter BloodCare facility has the capability to match patients with difficult transfusion needs and provide them blood products from our database of active donors with previously determined extended blood types. Our lab is accredited as an immunohematology lab by the Association for the Advancement of Blood and Biotherapies (AABB).
We thank the volunteer donors of the community blood supply for being there when we need them – their commitment to being repeat donors and honestly completing the donor questionnaire each and every time contributes to the current high levels of safety in our blood supply.
References
Infectious disease markers in autologous and directed donations. J Pink, A Thomson, B Wylie. Transfusion Medicine 1994; 4:135-138.
Markers for transfusion-transmitted disease in different groups of blood donors. JM Starkey, JL MacPherson, DC Bolgiano, ER Simon, TF Zuck, MH Sayers. JAMA 1989; 262(24):3452-3454.
Risk of hemolytic disease of the newborn as a result of directed donations from relatives. MH Kanter and SE Hodge. Transfusion 1989; 29:620-625.


